- Miracles – Desperate Patients see hopes from TCM in China
- Therapies in The Micro-invasive Osteopathy Hospital of TCM
- Medical Conditions treated in Micro-invasive Osteopathy Hospital
- Special Conditions treated in our hospital
- Are The Micro-Surgery and TCM treatments safe
- INPATIENT SERVICES
- OUTPATIENT TREATMENTS
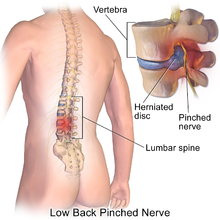
CHINESE TCM TREATMENT OF LUMBAR VERTEBRAL DISEASE
Chinese Medicine treatment is Acupuncture microsurgery which can even cure patients who relapsed after operations or failed in treatments by other surgeries. SEE the MIRACLES-Desperate Patients see hopes from TCM in China. By only localized anesthesia the “Inter-Vertebral Disc Rotation Surgery” is performed under X-ray locator to rotate intervertebral disc to loosen and separate nerves. This surgery reduces damage to the minimum, has no open cut, no removal of the inter-vertebral disc and is effective and painless. It uses a special rotational medical instrument to reach into the vertebral column and adjust the pressure on the inter-vertebral disc, and accurately separate the stuck parts to relieve pressure on the vertebral nerve. The whole surgery only takes about 30 minutes.
1. What is Slipped Disc
Slipped Disc, also called Spinal disc herniation, is a medical condition affecting the spine in which a tear in the outer, fibrous ring of an intervertebral disc allows the soft, central portion to bulge out beyond the damaged outer rings. Disc herniation is usually due to age-related degeneration of the outer ring, known as the anulus fibrosus, although trauma, lifting injuries, or straining have been implicated as well. Tears are almost always postero-lateral (on the back of the sides) owing to the presence of the posterior longitudinal ligament in the spinal canal.[1] This tear in the disc ring may result in the release of chemicals causing inflammation, which may directly cause severe pain even in the absence of nerve root compression.
Disc herniations are normally a further development of a previously existing disc protrusion, a condition in which the outermost layers of the anulus fibrosus are still intact, but can bulge when the disc is under pressure. In contrast to a herniation, none of the central portion escapes beyond the outer layers. Most minor herniations heal within several weeks. Anti-inflammatory treatments for pain associated with disc herniation, protrusion, bulge, or disc tear are generally effective. Severe herniations may not heal of their own accord and may require surgery. The condition is widely referred to as a slipped disc, but this term is not medically accurate as the spinal discs are firmly attached between the vertebrae and cannot "slip" out of place.
2. Symptoms
Symptoms of a herniated disc can vary depending on the location of the herniation and the types of soft tissue that become involved. They can range from little or no pain if the disc is the only tissue injured, to severe and unrelenting neck or lower back pain that will radiate into the regions served by affected nerve roots that are irritated or impinged by the herniated material. Often, herniated discs are not diagnosed immediately, as the patients come with undefined pains in the thighs, knees, or feet. Other symptoms may include sensory changes such as numbness, tingling, paresthesia, and motor changes such as muscular weakness, paralysis and affection of reflexes. If the herniated disc is in the lumbar region the patient may also experience sciatica due to irritation of one of the nerve roots of the sciatic nerve. Unlike a pulsating pain or pain that comes and goes, which can be caused by muscle spasm, pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body. It is possible to have a herniated disc without any pain or noticeable symptoms, depending on its location. If the extruded nucleus pulposus material doesn't press on soft tissues or nerves, it may not cause any symptoms. A small-sample study examining the cervical spine in symptom-free volunteers has found focal disc protrusions in 50% of participants, which suggests that a considerable part of the population can have focal herniated discs in their cervical region that do not cause noticeable symptoms.
A prolapsed disc in the lumbar spine can cause radiating nerve pain. This type of pain is usually felt in the lower extremities or groin area. Radiating nerve pain caused by a prolapsed disc can also cause bowel and bladder incontinence.
Typically, symptoms are experienced only on one side of the body. If the prolapse is very large and presses on the nerves within the spinal column or the cauda equina, both sides of the body may be affected, often with serious consequences. Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. This disorder is called cauda equina syndrome.
3. Diagnosis
Diagnosis is made by a practitioner based on the history, symptoms, and physical examination. Tests may be performed to confirm or rule out other causes of symptoms such as spondylolisthesis, degeneration, tumors, metastases and space-occupying lesions, as well as to evaluate the efficacy of potential treatment options.
Physical examination
The straight leg raise may be positive, as this finding has low specificity; however, it has high sensitivity. Thus the finding of a negative SLR sign is important in helping to "rule out" the possibility of a lower lumbar disc herniation. A variation is to lift the leg while the patient is sitting. However, this reduces the sensitivity of the test.
Imaging
X-ray: Although traditional plain X-rays are limited in their ability to image soft tissues such as discs, muscles, and nerves, they are still used to confirm or exclude other possibilities such as tumors, infections, fractures, etc. In spite of these limitations, X-ray can still play a relatively inexpensive role in confirming the suspicion of the presence of a herniated disc. If a suspicion is thus strengthened, other methods may be used to provide final confirmation.
CT or CAT scan: It can show the shape and size of the spinal canal, its contents, and the structures around it, including soft tissues. However, visual confirmation of a disc herniation can be difficult with a CT.
Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology. It can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and tumors. It shows soft tissues even better than CAT scans. An MRI performed with a high magnetic field strength usually provides the most conclusive evidence for diagnosis of a disc herniation. T2-weighted images allow for clear visualization of protruded disc material in the spinal canal.
Myelogram: An x-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces. By revealing displacement of the contrast material, it can show the presence of structures that can cause pressure on the spinal cord or nerves, such as herniated discs, tumors, or bone spurs. Because it involves the injection of foreign substances, MRI scans are now preferred for most patients. Myelograms still provide excellent outlines of space-occupying lesions, especially when combined with CT scanning (CT myelography).
Electromyogram and Nerve conduction studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves, and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury, or whether there is another site of nerve compression. EMG/NCS studies are typically used to pinpoint the sources of nerve dysfunction distal to the spine.
The presence and severity of myelopathy can be evaluated by means of Transcranial Magnetic Stimulation (TMS), a neurophysiological method that allows the measurement of the time required for a neural impulse to cross the pyramidal tracts, starting from the cerebral cortex and ending at the anterior horn cells of the cervical, thoracic or lumbar spinal cord. This measurement is called Central Conduction Time (CCT). TMS can aid physicians to:
determine whether myelopathy exists
identify the level of the spinal cord where myelopathy is located. This is especially useful in cases where more that two lesions may be responsible for the clinical symptoms and signs, such as in patients with two or more cervical disc hernias
follow-up the progression of myelopathy in time, for example before and after cervical spine surgery
TMS can also help in the differential diagnosis of different causes of pyramidal tract damage.
4. Treatments
Many minor disc herniations heal on their own with conservative treatment, but occasionally disc herniations require surgery for correction. A primary focus of surgery is to remove pressure or reduce mechanical compression on a neural element— either the spinal cord, or a nerve root. But it is increasingly recognized that back pain, rather than being solely due to compression, may also be due to chemical inflammation. This inflammatory molecule, called tumor necrosis factor-alpha (TNF), is released not only by the herniated disc, but also in cases of disc tear (annular tear), by facet joints, and in spinal stenosis. In addition to causing pain and inflammation, TNF may also contribute to disc degeneration.
 The majority of spinal disc herniation cases occur in the lumbar region (95% in L4-L5 or L5-S1).
The majority of spinal disc herniation cases occur in the lumbar region (95% in L4-L5 or L5-S1).
The second most common site is the cervical region (C5-C6, C6-C7). Initial treatment usually consists of non-steroidal anti-inflammatory pain medication (NSAIDs), but the long-term use of NSAIDs for people with persistent back pain is complicated by their possible cardiovascular and gastrointestinal toxicity.
Initial treatment usually consists of non-steroidal anti-inflammatory pain medication (NSAIDs), but the long-term use of NSAIDs for people with persistent back pain is complicated by their possible cardiovascular and gastrointestinal toxicity.
Epidural corticosteroid injections provide a slight and questionable short-term improvement in those with sciatica but are of no long term benefit. Complications occur in 0 to 17% of cases when performed on the neck and most are minor. In 2014, the US Food and Drug Administration (FDA) suggested that the "injection of corticosteroids into the epidural space of the spine may result in rare but serious adverse events, including loss of vision, stroke, paralysis, and death." and that "The effectiveness and safety of epidural administration of corticosteroids have not been established, and FDA has not approved corticosteroids for this use."
CHINESE MEDICINE TREATMENT OF CERVICAl VERTEBRAL DISEASE
Non-surgical treatments include physiotherapy, hand manipulation, medication, fixed or restricted neck movements, massage, acupuncture, needle-blade treatment, herbal medicine treatment, etc.Though these treatments have some positive effect, the disease can relapse easily and they have limited effect on patients with late-stage disease. Surgical treatment recommended are Acupuncture microsurgery.
CHINESE MEDICINE TREATMENT OF LUMBAR VERTEBRAL DISEASE
Lumbar Intervertebral Disc Protrusion is a frequent source of low back pain. Sciatica is defined as neuralgia along the course of the sciatic nerve. Whether spinal manipulation (ie, chiropractic care) improves the rate of recovery in patients with disc disease is controversial. Multiple surgical techniques have been used in patients with disc herniation who have not responded to conservative therapies. These therapies include diskectomy, spinal fusion, and injection of some chemicals. But these surgical treatments may bring big traumas. Acupuncture microsurgery is TCM treatment which has minimum damage and no open cut..
5. How Acupuncture-Microsurgery is performed
By only localized anesthesia the “Inter-Vertebral Disc Rotation Surgery” is performed under X-ray locator to rotate intervertebral disc to loosen and separate nerves. This surgery reduces damage to the minimum, has no open cut, no removal of the inter-vertebral disc and is effective and painless. It uses a special rotational medical instrument to reach into the vertebral column and adjust the pressure on the inter-vertebral disc, and accurately separate the stuck parts to relieve pressure on the vertebral nerve. The whole surgery only takes about 30 minutes.
Contact us for more details:
WhatsApp: +86 18032911295; Phone: +86 13230481935 Skype: cn.tcm.academy; Email : tcm-doctor@outlook.com
The Traditional Chinese Medicine Hospital was founded in 2006 with the purpose of bringing the benefits of Traditional Chinese Medicine (TCM) to Chinese and non-Chinese persons who seek Traditional Chinese Medicine as a cure for a variety of ailments which Western medicine had failed to remedy. Beginning with the modest staff, the hospital opened in Southeast Beijing and rapidly expanded its range of services and expertise.
Today, the hospital has a staff of 20 full-time doctors and 15 nurses, among a full-time staff numbering 60 people. In addition, the hospital also employs a compliment of visiting doctors and health professional who are available for medical consultations and treatments. The hospital offers a broad spectrum of treatments for oestoarthritic ailments, shoulder and knee conditions, chronic pain, chronic lower back problems, diabetes-related conditions, as well as neck and spinal conditions. In addition, our TCM Hospital is a recognized leader in the treatment of prostate care , pelvic disease, and gynecological conditions.
In-patient and out-patient treatments provided by the Hospital include acupuncture and electroacupuncture, masseotherapy, We also have an on-site, comprehensive pharmacy offering a full complement of Western and Chinese pharmaceutical products. In 2008, the hospital provided treatments to more than 500 foreign in-patients and additional 5,000 received outpatient services. In addition, we also operate two hospital clinics in Asia.
Beijing Traditional Chinese Medicine Hospital is dedicated to providing high-quality, cost-efficient services to its inpatient and outpatient communities. Our highly-trained staff provides first-rate, one-on-one care comparable to any other TCM hospital in Beijing. We welcome you to consult with our staff on your particular medical conditions.